72 year old female presents to HUM with shortness of breath and increasing lower extremity edema over the last month.
Vitals: SBP 160s, HR 170s, RR 26, O2 sat 94 % on RA
On exam, patient tachypneic, able to speak in short sentences, had irregular heart rate, crackles through lungs with decreased breath sounds bilaterally, distended abdomen with marked bilateral lower extremity edema.
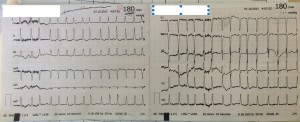
WHAT DOES HER EKG SHOW? (Below is a short video of her monitored rhythm.)
AXIS: Normal axis around +60 degrees (I+, II+, III+, AvL most isoelectric so axis must be 90 degrees away from -30 –> +60 – cannot be -120 because I is positive)
RATE: around 180 bpm
RHYTHM: IRREGULAR irregular (no pattern) without p waves
Interval: QRS narrow
SIZE: unremarkable
ST SEGMENTS: unremarkable
Remember, there is only ONE rhythm that Can be IRREGULARLY irregular, meaning irregular WITHOUT a pattern, and that’s atrial fibrillation.
On the video showing the monitored rhythm, you will see the HR bouncing back and forth between 150s – 180s. This kind of irregularity is almost always atrial fibrillation, so if you see a heart rate ever “bouncing around,” for example going quickly between 120s – 150s – think ATRIAL FIBRILLATION.
Patient placed on BIPAP, given nitroglycerine, lasix and started on amiodarone.
QUESTION: Why do you directly start with amiodarone? Was the AFib new, less than 7 days? Didn’t she have thrombus probe by transoesophageal Ultrasound ?
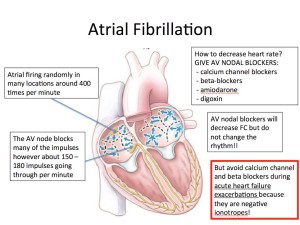
We could not determine if the Afib was new as she had no prior medical workups. Based on her systems, we believe she likely may have been in fib for the last month (when her symptoms but no real good way to know). We started with amiodarone because she was in an acute CHF exacerbation (pulmonary edema, dyspnea, mild hypoxia). Beta blockers and calcium channel blocker while great at blocking AV node and therefore decrease HR, are negative ionotropes and can decrease cardiac output. When using them in CHF patients, I prefer to stabilize them better (diuresis, decreasing preload with nitro, etc) prior to starting those medications. Amiodarone is not a negative ionotrope and therefore does not have the same risk. Digoxin would also be a good choice, it is actually a positive ionotrope and could increase cardiac output but does often take long to start working but would have been a fine choice as well.
As far as transesophageal US, we do not do that (yet) in Mirebalais, which does pose a problem especially because we do not have a good system for long term anticoagulation. When a patient is in afib with poorly organized atrial function, patient is at risk for developing an atrial clot which could embolize to the brain and cause a stroke. Therefore, it is recommended if patient is in atrial fibrillation for greater then 48 hours, time estimated where a clot can build up, we SHOULD not try to change the rhythm unless (shock), because there is a risk of patient throwing clot to brain, meaning risk greater than benefit, unless we can rule one out with a transesophageal echo (transthoracic echo which we can do in the ED not sensitive enough).
But if you have a reliable patient and symptoms started within 48 hours, electrical cardioversion is a great and SAFE option.
Our patient likely had afib for longer than 48 hours, therefore — I forgot to mention — we did start the patient on enoxaparin (low molecular weight heparin) for this reason (can use the CHADs score to determine who will benefit from anticoagulation). Typically, patient would either be on 4 weeks of anticoagulation OR recieve a transesophageal echo to rule out a atrial clot before RHYTHM change is considered (i.e. electrical cardioversion or antiarrythmics – flecainide, procainimide, etc). As we can therefore not rule out a clot, we initial RATE control with anticoagulation as opposed to RHYTHM control, and we chose amiodarone. Of note, to my knowledge, there is also no good evidence to suggest patient has improved mortality if put back in sinus as opposed to remained in rate controlled afib and appropriately anticoagulated.
But you do raise an important point. Since we cannot do a transesophageal echo OR easily do long term anticoagulation, is the patient at unnecessary risk remaining in afib, and is it possible that despite the risk of embolizing a clot, patient would be better off being electrically cardioverted in the ER even if they had been in afib for longer than 48hours? I do not know the answer to this question. But I will try to ask a cardiologist!