An 80 yr old male presented to the HUM ED complaining of acute onset epigastric and abdominal pain that started approximately 12 hours prior to arrival and was followed by multiple episodes of coffee ground emesis. Patient arrived to the ED holding his abdomen and screaming in pain.
Blood pressure: 100/60 Heart rate: 150 RR: 28 Saturation: 88% on non-rebreather
Abdominal exam revealed a rigid abdomen with significant rebound and involuntary guarding.
His FAST is below:
Patient received antibiotics, hydration, pain control, x-rays and a surgical consult. A foley was placed with 50cc of urine output. Our surgical team evaluated him and agreed that his presentation was consistent with a likely intra-abdominal perforation however patient’s condition was thought to be too unstable to operate with an operative mortality approaching 100%. 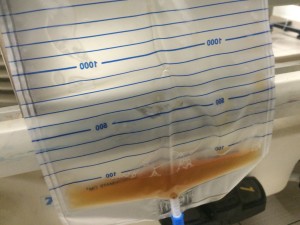 After 7 hours and 4L of normal saline, patient’s urine output was less than 100cc (pictured to the right), his heart rate remained in sinus in the 140s – 150s, his mental status began to decline and his blood pressure started to drop to a systolic in the 90s. He continued to move around the stretcher in significant pain.
After 7 hours and 4L of normal saline, patient’s urine output was less than 100cc (pictured to the right), his heart rate remained in sinus in the 140s – 150s, his mental status began to decline and his blood pressure started to drop to a systolic in the 90s. He continued to move around the stretcher in significant pain.
What must we do now to properly treat this patient?
The patient described above has an acute illness which cannot be reversed, but that does not mean he cannot be treated. While we could not treat the patient’s underlying disease, we can very effectively provide him comfort by treating his pain, and this we did by placing the patient on a morphine drip.
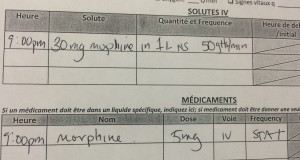
Patient was started on a morphine drip at approximately 5mg of morphine per hour (30mg of morphine in 1L of NS at 50 drops/min), and family was told to let us know if they felt the patient was still in pain, at which time we could give extra boluses of pain medication for further comfort. Family was counseled on the patient’s poor prognosis and reassured that we were doing everything we could to prevent suffering. Providing comfort care (to the patient AND the family) means treating discomfort, with medications and counseling, with the aggressiveness that we treat curable illness.
As emergency physicians, the truth is that we will be present at the end of many lives, and will be forced to be doctors to many patients who come with diseases we cannot cure and who will experience outcomes we cannot prevent. The high prevalence of irreversible illness in the emergency department is why all around the world, palliative and comfort care is rapidly becoming a fundamental part of emergency medical work.
In June 2012, the American College of Emergency Physicians published a Information Paper in order “to start the discussion of integrating the subspecialty of hospice and palliative care into everyday emergency medicine practice.” They note that “there is a growing body of literature focusing on palliative care in the ED and numerous champions of this subspecialitiy emerging in hospital of all sizes.” There are now many fellowships for emergency physicians in palliative care, and in the coming years, we are sure to see more to come.
As Emergency Physicians, we train in the hopes of saving lives and curing treatable illness. When this happens, it feels good and makes us feel accomplished. In the chaos of the Emergency Department, with so many needs waiting to be addressed, palliative and comfort care can easily be forgotten. Therefore we must always remind ourselves that providing attentive and compassion care for the dying is now recognized as one of our core responsibilities.