An 18 yr old female with a known history of mitral stenosis presents to the HUM ED with two weeks of shortness of breath and chest discomfort.
This is her EKG. What does it show?
HINT: 15 minutes later, after approx 500cc of NS, here is a look at her monitor, how does this help us?
BIGGER HINT: Below is a video of us giving the patient 6mg of adenosine.
So what does her EKG show?
RATE: 141 BPM
AXIS: Slight right axis deviation (I-, II +, III+). Axis approximately +120 degrees (most isoelectric lead AvR, -150 degrees, axis must be approximately 90 degrees from most isoelectric lead, with I being negative, axis must be around +120 degrees).
RHYTHM: Regular w/ p waves always followed by QRS complex, QRS complex always preceded by P wave
INTERVAL: QRS narrow
SIZE: normal
ST SEGMENTS: unremarkable
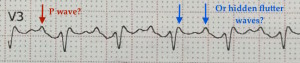
Upon initially viewing this EKG, you might be inclined to believe that this is sinus rhythm because in some leads, especially lead V3, there is a deflection that looks very similar to a “p-wave.” But is this a true p-wave coming from the sinus node, or is this actually a flutter wave that just looks like a “p-wave?”
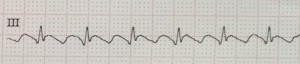
These are actually flutter waves that can easily be mistaken for p-waves of sinus node origin if the EKG is not closely examined. The waves in Lead III however do more closely resemble typical flutter waves:
So how can sure that this is atrial flutter? Placing this patient on a monitor and watching that monitored rhythm almost confirms that this is NOT sinus rhythm. Sinus rhythm will always have some variation, both beat to beat with breathing, and over time with interventions like pain control and fluids.  Sinus rhythm does not stay on one number for a long time, and so watching this monitored rhythm, in which “141” is the constant rate, you should immediately suspect that this is not a sinus rhythm.
Sinus rhythm does not stay on one number for a long time, and so watching this monitored rhythm, in which “141” is the constant rate, you should immediately suspect that this is not a sinus rhythm.
So now, after closely examining the EKG and watching the monitored rhythm, we are almost completely sure this is not sinus, but how can we confirm the diagnosis of atrial flutter with 100% certainty? We can temporarily block the AV node and look for flutter waves, which is what you see in the second video.
Remember that while blocking the AV node has a good chance of stopping SVT, it will not change the underlying rhythm if the patient is in atrial flutter. 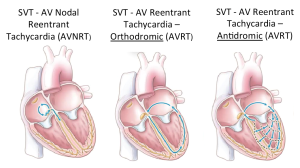 In every type of SVT, the abnormal electrical conduction is looping through the AV node. Therefore, blocking the AV node stops the abnormal rhythm and give the sinus node the time it needs to restart.
In every type of SVT, the abnormal electrical conduction is looping through the AV node. Therefore, blocking the AV node stops the abnormal rhythm and give the sinus node the time it needs to restart. 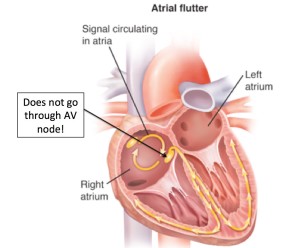 In atrial flutter however, the abnormal current is not going through the AV node, so blocking the AV node will not stop the “flutter” in the atria, it will only stop the conduction to the ventricles and you will be able to see flutter waves without ventricular conduction until the av node becomes unblocked and the ventricular conduction and QRS complexes return. The sinus node can also be temporarily blocked with any maneuver that produces vagal stimulation including carotid sinus massage, valsalva maneuvers, or placing an ice pack or ice cold cloth on an infants face, and these actions, if successful, will have the same effect on the observed rhythm.
In atrial flutter however, the abnormal current is not going through the AV node, so blocking the AV node will not stop the “flutter” in the atria, it will only stop the conduction to the ventricles and you will be able to see flutter waves without ventricular conduction until the av node becomes unblocked and the ventricular conduction and QRS complexes return. The sinus node can also be temporarily blocked with any maneuver that produces vagal stimulation including carotid sinus massage, valsalva maneuvers, or placing an ice pack or ice cold cloth on an infants face, and these actions, if successful, will have the same effect on the observed rhythm. 
This is very important, because while this EKG and monitor highly suggest atrial flutter, in the future you will encounter a patient where the EKG is even less clear, and in order to determine the underlying rhythm and treat the patient appropriately, you will need consider blocking the AV node. Do remember that patients in sinus tachycardia with a temporary AV blockade will also have a transient slowing of the ventricular rate but without the evidence of flutter or fibrillation waves during the AV blockade.
While adenosine is quite effective, short-acting and safe for the management of tachyarrythmias in the ED, it can be quite uncomfortable to the patient, so make sure you warn the patient before hand that they will briefly feel some chest discomfort. Emphasize that it will be very brief and that it is not dangerous and is very useful to diagnose (if the patient has atrial flutter or atrial fibrillation) and to treat (if the patient has SVT) their abnormal cardiac rhythm. You do not need to sedate a patient for this procedure, but you must reassure them. Do take precautions and always have a defibrillator by the bedside during this procedure. While you likely will never need to use it because ventricular arrhythmias after adenosine administration are extremely rare, there are reports of them occurring and should you be one of rare unlikely physicians to witness this, you do not want to be caught off guard.
Also do consider the other less uncomfortable interventions which can be quite effective. One recent study in the Lancet found that a modified vagal maneuver for emergency treatment of SVT could convert patients from SVT to sinus rhythm 43% of the time and argues that this method should be considered as a routine first treatment.
But most importantly, whatever method you choose, you cannot manage a tachyarrhythmia if you are tricked into believing it is a sinus rhythm, so always remember if someone remains usually tachycardic for an unknown reason in the ED, there are two things that you MUST do:
- closely reexamine the EKG
- watch the monitored rhythm over time
Lastly, while respecting our patients and knowing our medicine are the most important things in our profession, knowing our equipment is not far behind. Below is a quick video of our first attempt, watch and enjoy:
More information:
EB medicine: Management of specific tachyarrythmias
Life in the Fast Lane – Atrial Flutter


this is my favorite rhythm!!
So helpful to have it all explained. Thanks!